Drug resistance: Patients with infections no longer responding to treatment, say experts
Medical professionals have warned that antibiotic resistance is having a negative impact on Nigerian patients and healthcare delivery.
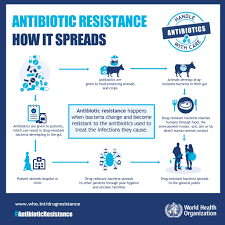
According to the World Health Organisation, antimicrobial resistance (AMR) happens when bacteria, viruses, fungi, and parasites alter over time and stop responding to medications, making illnesses more difficult to treat and raising the risk of disease spread, serious illness, and death. Consequently, the medications lose their efficacy and the diseases continue within the body, raising the possibility of spreading to other people.
Antimicrobials are drugs that are used to prevent and treat infections in people, animals, and plants. They include antibiotics, antivirals, antifungals, and antiparasitics. Superbugs are microorganisms that have developed resistance to antibiotics.
According to UN estimates, bacterial AMR directly caused 1.27 million deaths worldwide in 2019 and indirectly caused 4.95 million fatalities.
According to World Bank projections, AMR might cause $1 trillion in additional healthcare expenses by 2050 and $1 trillion to $3.4 trillion in annual losses in gross domestic product by 2030.
Children and other vulnerable groups are particularly at risk of contracting diseases that are resistant to treatment, according to a recent research by the Africa Centres for Disease Control and Prevention.
According to the research, "the continent faces the highest antimicrobial resistance mortality rate, with 27.3 deaths per 100,000—exceeding the combined death toll from HIV-AIDS, tuberculosis, and malaria."
According to the research, Africa has a disproportionately high burden of infectious illnesses; it accounts for 25% of worldwide tuberculosis deaths, 70% of HIV-positive individuals, and 95% of malaria deaths.
according to Dr. Oladipo Kolawole, a medical virologist and immunologist at Adeleke University in Ede, Osun State, is putting an increasing amount of strain on healthcare systems across the globe.
According to Kolawole, AMR increases the chance of serious consequences or death, lengthens sickness, increases healthcare expenses, and results in inefficient therapies.
"As a result, healthcare prices have gone up: It costs more to treat infections that are resistant to drugs. Patients frequently need more intense treatment, lengthier hospital stays, and the administration of newer, priciest antibiotics as a last option. AMR is linked to increased mortality and problem risks. infections that were once easily treatable, such as pneumonia, tuberculosis, and sepsis, are now becoming life-threatening due to resistance.
Additionally, resistant infections have the ability to spread throughout healthcare facilities and communities, resulting in outbreaks that are challenging to contain and demand a large amount of public health resources. The efficacy of organ transplants, cancer treatments, and surgery is threatened by AMR. The safety and success rates of these treatments are jeopardised due to the growing resistance to the efficient antibiotics used to prevent and treat infections.
AMR has the potential to reverse decades of medical advancement. Rising resistance threatens the foundation of many elements of healthcare, which is the ability to treat infections. Furthermore, AMR is a worldwide health concern that necessitates concerted international efforts to address through research, surveillance, and novel treatments because it knows no geographical bounds, the speaker added.
Tanimola Akande, a former National Chairman of the Association of Public Health Physicians of Nigeria and a professor of public health at the University of Ilorin, underlined that antibiotic-resistant microorganisms (AMR) are bacteria that have developed resistance to antibiotics that are intended to eliminate them within the human system.
According to him, when bacteria develop resistance, they remain viable even when treated with the specific antibiotics to which they have become resistant.
This could result in the illness's symptoms and indicators worsening and possibly even fatality. It may lengthen hospital stays and the length of antibiotic treatments, incurring expenditures for patients both directly and indirectly.
"A stronger antibiotic or a combination of antibiotics must be administered to kill the germs when antibiotic-resistant bacteria (AMR) develops. These antibiotics are typically more expensive. When existing antibiotics lose their effectiveness, newer, more costly ones must be created, Akande emphasised.